“When joint pain is severe and interferes with daily activities, work and sleep, joint replacement may be an option”
The Hip
If you're experiencing hip problems, the team at Sydney Orthopaedic Consultants can help get you back to living the life you want. We provide individualised treatment plans and use advanced techniques to get you on the road to recovery as soon as possible.
Hip Conditions
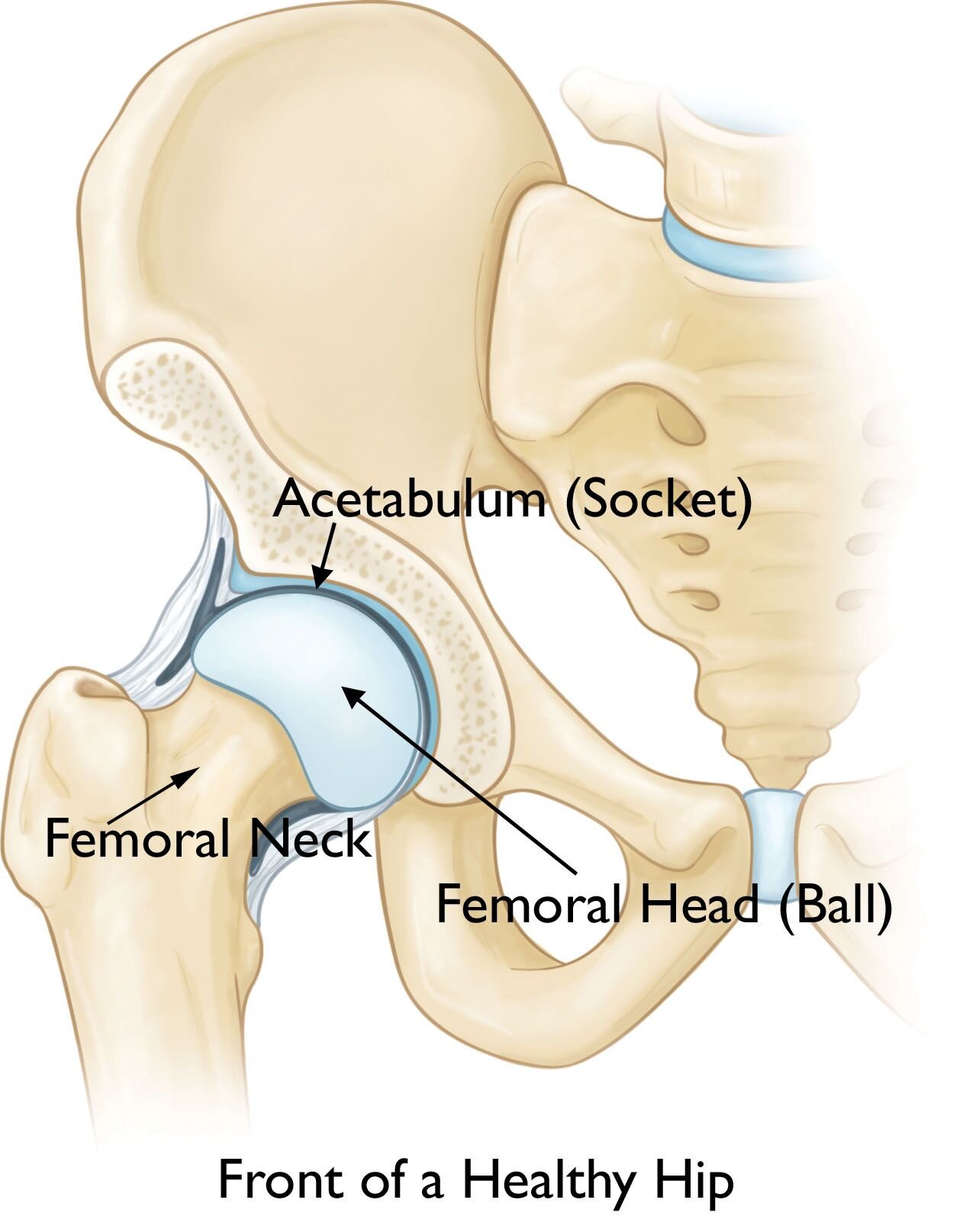
Anatomy of the Hip
The hip is one of the most important joints in the human body. It bears our body weight while we sit, stand, walk, and run. It is extremely flexible, and allows for a large range of motion while providing great stability.
Image © American Academy of Orthopaedic Surgeons.
The hip is a simple ball and socket joint. Normally, the parts of the hip joint work together and the joint moves easily without pain. However; disease, arthritis, or injury can disturb the normal function of the hip joint. This can result in hip pain, groin pain, muscle weakness, and limited movement. Longer life expectancies and greater activity levels as people age have lead to joint replacements being performed in greater numbers of patients.
Hip Bones
There are two main bone structures that make up the hip.
Femoral head a ball shaped piece of bone at the top of the femur.
Acetabulum the cup-like socket in the pelvis that the femoral head fits into.
Tissues
There are several types of tissue in the hip joint.
Cartilage Both the femoral head and the acetabulum are lined with cartilage. Cartilage creates a smooth surface for the bones to glide over one another without friction and acts as a shock absorber in high impact activities.
Synovium thin membrane called synovium exists between the femoral head and the acetabulum. It produces fluid which lubricates the joint and adds additional cushioning to support smooth movement.
Ligaments Bands of fibrous tissue known as ligaments hold the femoral head in the acetabulum. The purpose of these ligaments is to hold the femoral head in place and to increase stability.
Muscles and tendons large muscles surround the hip to add further support and enable movement. Tendons connect the muscles to the bones.
Movements
The ball and socket function of the hip joint ensures a wide range of movement of the lower limbs.
Flexion is the movement of lifting your leg out in front of you.
Extension is the movement of lowering your lifted or moving your leg behind you.
Adduction is the movement of lifting your leg inward to cross your leg over the midline in front of you
Abduction is the movement of lifting your leg out to the side
Rotation is the the movement of turning your leg clockwise and anticlockwise.
Circumduction is the circular movement produced by moving your leg in an arc.
Hip Arthritis
If you have hip problems, the experienced and specialised team at Sydney Orthopaedic Consultants will provide you with an individualised treatment plan using the most advanced techniques available to help you quickly get back to living the life you want.
Arthritis is a general term that describes a number of conditions that result from inflammation of a joint. There are several types of arthritis that affects the hip joint.
Osteoarthritis is the most common form of hip arthritis and results from the wearing away of cartilage between the top of the thigh bone (femoral head) and the hip socket (acetabulum) causing the two bones to rub against each other and create friction on movement.
Rheumatoid arthritis is an autoimmune disease that causes swelling of the membrane lining of the joint (synovial membrane). The synovial membrane normally functions to increase cushioning and allow smooth movement between the femoral head and the acetabulum. The diseased synovial membrane caused by rheumatoid arthritis damages the cartilage lining the joint, and produces excess fluid in the joint leading to pain and poor movement.
Post traumatic arthritis develops following injury or fracture to the hip joint and results in pain and stiffness of the joint.
What are the symptoms?
Hip pain – may be felt in hip, groin, buttock, thigh or knee
Hip stiffness
Decreased range of hip movement
Swelling/inflammation
What are the causes?
OSTEOARTHRITIS AND POST TRAUMATIC ARTHRITIS
Osteoarthritis is the most common type of arthritis. As we age, the chances of developing arthritis increases, though the severity of the disease is different for everyone. People in early stages of life can also develop osteoarthritis.
Osteoarthritis breaks down the cartilage in joints and can occur in almost any joint in the body, though it occurs most often in the hips, knees and spine. Cartilage is the cushion that covers the ends of bones in normal joints and helps provide protection so those bones don’t rub together. it also serves as a shock absorber as wear and tear occurs in the joints after years of use. The cartilage can also be damaged by injuries or fractures to the joints resulting in post traumatic arthritis.
Risk factors for developing hip osteoarthritis include:
Being overweight
Increasing age
Previous hip fracture or injury
Family history of osteoarthritis
Repetitive stress on the joint through work or sport
Genetic defects in cartilage or improper formation of the hip joint at birth
RHEUMATOID ARTHRITIS
As rheumatoid arthritis is an autoimmune disease, the exact cause of is not known however family history and environmental factors are thought to be risk factors to the disease developing.
How is it diagnosed?
If you are experiencing the symptoms listed above, you should consult your doctor. Your doctor will take a detailed history of your pain and other symptoms, and your family medical history. A physical examination will also be undertaken to assess your range of hip movement, level of joint stiffness and gait (walking).
If your doctor suspects hip arthritis is the cause of your symptoms, you will be referred for a hip x-ray. A magnetic resonance imaging (MRI) scan or computed tomography (CT) scan may also occasionally be required. If rheumatoid arthritis is suspected, your doctor may also do a blood test to look for autoimmune factors that will be present in the blood.
There is no cure for arthritis, however there are treatment options to increase mobility and relieve pain.
NON SURGICAL:
Mild forms of osteoarthritis or osteoarthritis in its initial stages may be managed with a range of non-surgical options. These include:
Lifestyle modifications that include:
Weight loss
Reducing high-impact activities
Physiotherapy
Regular exercise as determined by your physiotherapist
Medication:
To manage pain
To reduce inflammation
SURGICAL:
Once your symptoms can no longer be managed with non-surgical treatment options and you are no longer able to undertake your usual daily activities, your doctor may recommend hip surgery. The type of surgery your doctor recommends will be determined in consultation with you based on your specific symptoms and risk factors.
Hip resurfacing involves removal of the damaged bone and cartilage of the femur and acetabulum and replaced with a smooth metal covering to decrease friction
Total hip replacement involves removing the entire femoral head (ball of the thigh bone that sits within the hip socket) and replacing it with a prosthetic femoral head that sits within a prosthetic hip socket.
Hip Treatments
Hip Resurfacing
Patients with advanced arthritis of the hip may be candidates for either traditional total hip replacement (arthroplasty) or hip resurfacing (hip resurfacing arthroplasty). Each of these procedures is a type of hip replacement, but there are important differences. Your orthopaedic surgeon will talk with you about the different procedures and which operation would be best for you.
Image © American Academy of Orthopaedic Surgeons.
In a traditional total hip replacement, the head of the thighbone (femoral head) and the damaged socket (acetabulum) are both removed and replaced with metal, plastic, or ceramic components.
In hip resurfacing, the femoral head is not removed, but is instead trimmed and capped with a smooth metal covering. The damaged bone and cartilage within the socket is removed and replaced with a metal shell, just as in a traditional total hip replacement.
Advantages of Hip Resurfacing
The advantages of hip resurfacing over traditional total hip replacements is an area of controversy among orthopaedic surgeons. Research is currently being done on this topic.
Hip resurfacings may be easier to revise. Because the components (called implants) used in hip replacements and hip resurfacings are mechanical parts, they can — and do — wear out or loosen over time. This typically occurs between 15 and 20 years after the procedure, although implants may last longer or shorter periods of time.
If an implant fails, an additional operation may be necessary. This second procedure is called a revision and it can be more complicated than the initial operation. Because hip resurfacing removes less bone from the femur (thighbone) than a traditional hip replacement, many surgeons believe it is easier to exchange implants that fail after hip resurfacing.Decreased risk of hip dislocation. In hip resurfacing, the size of the ball is larger than in a traditional hip replacement, and it is closer to the size of the natural ball of your hip. Because of this, it may be harder to dislocate. This stance is controversial because several factors can affect the risk of dislocation, such as surgical approach, and the type and size of the implants used.
More normal walking pattern. Some studies have shown that walking patterns are more natural following hip resurfacing compared to traditional hip replacement. These differences in walking are quite subtle, however, and special instruments are needed to measure them.
Candidates for Surgery
Unlike hip replacement, hip resurfacing is not suitable for all patients. Generally speaking, the best candidates for hip resurfacing are younger (less than 60), larger-framed patients (often, but not always male) with strong, healthy bone. Patients that are older, female, smaller-framed, with weaker or damaged bone are at higher risk of complications, such as femoral neck fracture.
A comprehensive evaluation by your orthopaedic surgeon will help you determine if you are a good candidate for hip resurfacing.
Anterior Hip Replacement
The main difference between anterior hip replacement and traditional hip replacement is the location of the surgical incision. The location of the incision determines which muscles will be cut or pushed aside during surgery.
Anterior hip replacement involves an incision at the font of the hip (the word anterior means “front”).
More traditional hip replacements use incisions at either the side of the hip (lateral incision) or the back of the hip (posterior incision).
Description
The anterior approach to hip replacement is a minimally invasive surgical technique in which surgeons makes an incision at the front of the hip instead of through the buttocks or side of the hip and work between the muscles to keep them intact, rather than cutting through them, which is common with traditional hip replacement.
The reason anterior hip replacement is considered less invasive is because it involves little to no muscle cutting. Over time, experts have learned that it is not the length of the incision that affects recovery. Instead, what matters is the amount of damage to muscles and other soft tissues during surgery. Less muscle cutting is associated with a faster, less painful recovery.
The goal of using shorter incisions or changing the location of the incision is to reduce pain and speed recovery. Minimally invasive techniques may not, however, be suitable for all patients. Your orthopaedic surgeon will discuss different surgical options with you.
TRADITIONAL HIP REPLACEMENT
To perform a traditional hip replacement:
The surgeon makes a 10- to 12-inch incision on the side of the hip, then splits or detaches the muscles from the hip, allowing the hip to be dislocated and fully viewed.
The surgeon removes the damaged femoral head and inserts a metal stem into the hollow center of the femur. The surgeon then places a metal or ceramic ball on the upper part of the stem. This ball replaces the damaged femoral head that was removed.
The surgeon removes the damaged cartilage surface of the socket (acetabulum) and replaces it with a metal socket. The surgeon may use screws or cement to hold the socket in place.
The surgeon inserts a plastic, ceramic or metal spacer between the new ball and the socket to allow for a smooth gliding surface.
MINIMALLY INVASIVE HIP REPLACEMENT
Small-incision surgery using the posterior, lateral, or anterolateral approach.
For this type of minimally invasive hip replacement, the surgeon uses a single incision that usually measures 3 to 6 inches. The length of the incision depends on the size of the patient and the difficulty of the procedure.
The surgeon makes the incision on the side or back of the hip. The muscles and tendons are split or detached from the hip, but to a lesser extent than in traditional hip replacement surgery. They are routinely repaired after the surgeon places the implants. This encourages healing and helps prevent dislocation of the hip.
Multiple-incision surgery
Some surgeons perform a hip replacement through two separate small incisions. The concept behind two incisions is to approach the pelvis (cup) through one incision and the femur (thighbone) through a separate incision.
Approaching the hip in this manner may allow for less disruption of the underlying tissues compared to using one incision.
For this procedure, surgeons often use X-ray guidance during surgery to ensure proper placement of the implants.
MINIMALLY INVASIVE SURGERY BASED ON INCISION LOCATION
Direct anterior approach
Another approach to minimally invasive surgery is to change the location of the incision. In the past decade, the direct anterior approach has become popular because it requires less disruption of the underlying tissue and muscle.
In this approach, the surgeon makes the incision on the front of the hip.
Less cutting of the muscle is necessary, and recovery has been reported to be faster.
The anterior approach is often performed with the use of a special operative table and instruments.
As with traditional hip replacement surgery, after minimally invasive hip replacement, you will either go home the same day or spend 1 to 3 days in the hospital.
Physical rehabilitation is a critical component of recovery. Your surgeon or a physical therapist will provide you with specific exercises to help increase your range of motion and restore your strength.
Candidates for Minimally Invasive Total Hip Replacement
Minimally invasive total hip replacement is not suitable for all patients. Your doctor will conduct a comprehensive evaluation and consider several factors before determining whether the procedure is an option for you.
In general, candidates for minimal incision procedures are thinner, younger, healthier, and more motivated to participate in the rehabilitation process, compared with patients who undergo the traditional surgery.
Minimally invasive techniques may be less suitable or create a higher risk of complications for patients who:
Are overweight
Have already undergone other hip surgeries
Have a significant deformity of the hip joint
Are very muscular
Have health problems that may slow wound healing
Like traditional hip replacement surgery, minimally invasive surgery should be performed by a well-trained, highly experienced orthopaedic surgeon. Your orthopaedic surgeon can talk to you about their experience with minimally invasive hip replacement surgery, and the possible risks and benefits of the techniques for your individual treatment.
Total Hip Replacement
Whether you have just begun exploring treatment options or have already decided to undergo hip replacement surgery, this information will help you understand the benefits and limitations of total hip replacement. This article describes how a normal hip works, the causes of hip pain, what to expect from hip replacement surgery, and what exercises and activities will help restore your mobility and strength, and enable you to return to everyday activities.
TOTAL HIP REPLACEMENT VIDEO:
The animation below visually guides you through the process of a total hip replacement, a surgical procedure in which parts of an arthritic or damaged hip joint are removed and replaced with a metal, plastic or ceramic device called a prosthesis.
Video / Animation © Visual Health Solutions, Inc.
If your hip has been damaged by arthritis, a fracture, or other conditions, common activities such as walking or getting in and out of a chair may be painful and difficult. Your hip may be stiff, and it may be hard to put on your shoes and socks. You may even feel uncomfortable while resting.
If medications, changes in your everyday activities, and the use of walking supports do not adequately help your symptoms, you may consider hip replacement surgery. Hip replacement surgery is a safe and effective procedure that can relieve your pain, increase motion, and help you get back to enjoying normal, everyday activities.
What is a Total Hip Replacement?
Total hip replacement is exactly that – a surgical procedure designed to replace the components of this hard-working joint. Replacing the original ball and socket joint. The hip socket (acetabulum) is replaced with an artificial cup and liner, and the upper thigh bone is replaced with an artificial stem and new ball (femoral head). It is an excellent procedure designed to improve pain relief, motion and function. Patients report returning to their active lifestyles, with no pain. On average, hip implants last 20 years or more.
When Surgery Is Recommended
There are several reasons why your doctor may recommend hip replacement surgery. People who benefit from hip replacement surgery often have:
Hip pain that limits everyday activities, such as walking or bending
Hip pain that continues while resting, either day or night
Stiffness in a hip that limits the ability to move or lift the leg
Inadequate pain relief from anti-inflammatory drugs, physical therapy, or walking supports
HIP X-RAY HEALTHY / UNHEALTHY
In this x-ray of a normal hip, the space between the ball and socket indicates healthy cartilage.
This x-ray of an arthritic hip shows severe loss of joint space.
Candidates for Surgery
There are no absolute age or weight restrictions for total hip replacements.
Recommendations for surgery are based on a patient's pain and disability, not age. Most patients who undergo total hip replacement are age 50 to 80, but orthopaedic surgeons evaluate patients individually. Total hip replacements have been performed successfully at all ages, from the young teenager with juvenile arthritis to the elderly patient with degenerative arthritis.
THE ORTHOPAEDIC EVALUATION
An evaluation with an orthopaedic surgeon consists of several components.
Medical history. Your orthopaedic surgeon will gather information about your general health and ask questions about the extent of your hip pain and how it affects your ability to perform everyday activities.
Physical examination. This will assess hip mobility, strength, and alignment.
X-rays. These images help to determine the extent of damage or deformity in your hip.
Other tests. Occasionally other tests, such as a magnetic resonance imaging (MRI) scan, may be needed to determine the condition of the bone and soft tissues of your hip.
Revision Hip Replacement
Total hip replacement is one of the most successful procedures in all of medicine. In the vast majority of cases, total hip replacement enables people to live more active lives without debilitating hip pain. Over time, however, a hip replacement can fail for a variety of reasons. When this occurs, your doctor may recommend that you have a second operation to remove some or all of the parts of the original prosthesis and replace them with new ones. This procedure is called revision total hip replacement.
Although both procedures have the same goals—to relieve pain and improve function and quality of life—revision surgery is different than primary total hip replacement. Revision hip replacement is a longer, more complex procedure. It requires extensive planning, as well as the use of specialised implants and tools, in order to achieve a good result.
(Left) Primary total hip replacement.
(Right) Revision total hip replacement.
Image © American Academy of Orthopaedic Surgeons.
Description
During primary total hip replacement surgery, the hip joint is replaced with an implant or prosthesis made of metal, plastic, and/or ceramic components. Although most total hip replacements are very successful, problems can develop over time. These problems may require a revision procedure to replace the original components.
There are different types of revision surgery. In some cases, only some components of the prosthesis need to be revised. In other cases, the whole prosthesis needs to be removed or replaced and the bone around the hip needs to be rebuilt with augments (metal pieces that substitute for missing bone) or bone graft.
Damage to bone and soft tissue around the hip may make it difficult for the doctor to use standard primary hip implants for revision hip replacement. In most revisions, the doctor will use specialised implants that are designed to compensate for the damaged bone and soft tissue.
The space around the femoral stem indicates that the component has loosened from the underlying bone.
Image © American Academy of Orthopaedic Surgeons.
An antibiotic spacer placed in the hip joint during the first stage of treatment for joint replacement infection.
Image © American Academy of Orthopaedic Surgeons.
When Revision Total Hip Replacement Is Recommended
IMPLANT WEAR AND LOOSENING
In order for a total hip replacement to function properly, an implant must remain firmly attached to the bone. During the initial surgery, the hip replacement components were either cemented into place or were "press fit" into the bone to allow bone to grow onto them. Sometimes, however, bone may fail to grow onto press-fit components. In addition, cemented or press-fit components that were once firmly fixed to the bone can eventually loosen, resulting in a painful hip.
The cause of loosening is not always clear, but repetitive high-impact activities, excessive body weight, and wear of the plastic liner between the ball and the metal cup are all factors that may contribute.
In addition, patients who are younger when they undergo the initial hip replacement may "outlive" the life expectancy of their artificial hip. For these patients, there is a higher long-term risk that revision surgery will be needed due to loosening or wear.
Infection
Infection is a potential complication of any surgical procedure, including total hip replacement. Infection occurs when bacteria attach in and around the surface of the prosthesis. Infection may occur while you are in the hospital or after you go home. It may even occur years later.
If a total hip replacement becomes infected, it can be painful and the implant may begin to lose its attachment to the bone. Even if the implant remains properly fixed to the bone, there may still be pain, instability, and drainage from the infection. Because bacteria cannot be easily eliminated from a joint replacement with antibiotics alone, revision surgery is usually necessary.
Revision surgery for infection can be done in different ways. To determine which procedure is best for you, your doctor will consider a number of factors, including:
The type of bacteria
The duration and severity of the infection
Your preference for a specific treatment
Debridement. In this procedure, your doctor will open up your hip, wash out the bacteria, and exchange the ball and plastic liner. The metal implants that are firmly attached to the bone are left in place. After debridement, you will receive intravenous antibiotics for several weeks to help cure the infection.
Staged surgery. In some cases, the implants must be completely removed. If the implants are removed to treat the infection, your doctor will usually perform the revision in two separate surgeries.
In the first surgery, your doctor will remove the implants and place a temporary cement spacer in your hip. This spacer is treated with antibiotics to help fight the infection and will remain in your hip for several weeks. During this time, you will also receive intravenous antibiotics.
When the infection has been cleared, your doctor will perform a second surgery to remove the antibiotic spacer and insert a new prosthesis. In general, removing the implant leads to a higher chance of curing the infection, but is associated with a longer recovery.
In some cases, your doctor may be able to remove the implants, wash out the hip, and place a new prosthesis all in the same operation. This procedure, which is called a one-stage exchange, may be appropriate in limited situations.
Recurrent Dislocation
A hip replacement has a ball-and-socket structure like that of your natural hip. For a hip replacement to work well, the ball must remain inside the socket. Trauma or certain hip positions can sometimes cause the ball to become dislodged from the socket. This is called a "hip dislocation." If you experience recurrent hip dislocations, you may need revision surgery to better align your hip joint or to insert a special implant designed to prevent dislocations.
Fracture
A periprosthetic fracture is a broken bone that occurs around the components of an implant. These fractures are most often the result of a fall, and often require revision surgery. To determine whether a revision is needed, your doctor will consider several factors, including the amount of remaining bone, whether your implant is loose, and the location of the fracture.
In rare circumstances, an implant itself can break. This also requires revision surgery.
Reaction to Metal Ions and Allergy to Metal
Over time, the metals used in implants can break down or wear, causing tiny particles to fall off the device into the space around the implant. This is more common with "metal-on-metal" devices, in which both the ball and socket components are made of metal. In some patients, sensitivity to the metal ions in these particles can result in damage to the bone and soft tissues around the hip and lead to the need for revision surgery.
In very rare cases, a patient allergy to the metal used in implants may cause pain around the site of the implant. There is no definitive agreement among doctors regarding metal allergy in this setting, however, and more studies are needed.
Other Factors
The likelihood of needing revision hip replacement is also impacted by individual differences among patients. For example, patients who are younger and more active are more likely to experience issues related to implant wear. Patients who have certain medical conditions, such as obesity or diabetes, and those who have had certain surgical procedures in the past, are more likely to experience infection or implant failure.
For more details on a revision hip replacement VISIT ORTHO INFO.
Treatment of Hip Femur Fractures
Image © American Academy of Orthopaedic Surgeons.
A hip fracture is a break in the upper portion of the femur (thighbone). Most hip fractures occur in elderly patients whose bones have become weakened by osteoporosis. When a hip fracture occurs in a younger patient, it is typically the result of a high-energy event, such as a fall from a ladder or vehicle collision.
Hip fractures can be very painful. For this reason, prompt surgical treatment is recommended. Treating the fracture and getting the patient out of bed as soon as possible will help prevent medical complications such as bed sores, blood clots, and pneumonia. In very old patients, prolonged bed rest can also lead to disorientation, which makes rehabilitation and recovery much more difficult.
Description
A hip fracture can cause injury to one of four areas of the upper femur:
Femoral head. The ball of the femur that sits in the socket. These are extremely rare and are usually the result of a high-velocity event.
Femoral neck. The area of the femur below the ball (femoral head).
Intertrochanteric area. The area below the neck of the femur and above the long part or shaft of the femur. It is called Intertrochanteric because it is marked by two bony landmarks: the greater trochanter and the lesser trochanter. These are the most common types of hip fracture.
Subtrochanteric area. The upper part of the shaft of the femur below the greater and lesser trochanters.
Cause
Most hip fractures result from low-energy falls in elderly patients who have weakened or osteoporotic bone. In these patients, even a simple twisting or tripping injury may lead to a fracture.
In some cases, the bone may be so weak that the fracture occurs spontaneously while someone is walking or standing. In this instance, it is often said that “the break occurs before the fall.” Spontaneous fractures usually occur in the femoral neck.
Stress fractures or fractures from repeated impact may also occur in the femoral neck. These fractures are often seen in long distance runners, particularly military recruits in basic training. When stress fractures occur in the subtrochanteric region of the hip, they are usually associated with prolonged use of certain osteoporosis medications.
Fractures of the femoral head are rare and are usually the result of a high-impact injury or are part of a fracture dislocation of the hip.
Imaging Scans
X-RAY
X-ray Scans
X-rays provided images of dense structures, such as bone. Most hip fractures can be diagnosed with an x-ray.
MRI Scans
Magnetic resonance imaging (MRI) scans. An MRI scan provides fine images of both soft tissue structures and bone. Because it is very sensitive, it can sometimes detect a small or incomplete fracture that cannot be seen on an x-ray.
CT Scans
Computerized tomography (CT) scans. A CT scan will provide a detailed cross-sectional image of your hip. Your doctor may order a CT scan to learn more about your fracture.
Treatment
Computerised tomography (CT) scans. A CT scan will provide a detailed cross-sectional image of your hip. Your doctor may order a CT scan to learn more about your fracture.
Most hip fractures require surgical treatment within 1 to 2 days of injury. Only a very small group of nondisplaced fractures in healthy patients can be treated without surgery, while a separate small group of patients may be too sick to safely have surgery.
Surgical treatment is required to relieve the acute pain of the fracture and to allow the patient to get out of bed. Having surgery as soon as possible can lessen the risk of complications.
This process of getting a patient medically ready for surgery is called optimisation. Ideally, it should be done within 48 hours, but sometimes it may take longer. Even if it does takes longer, it is better to be optimised than to rush to surgery.
Treatment for a hip fracture depends upon the type and location of the fracture, as well as the age and condition of the patient.