“From supporting the body’s weight, to squatting, pivoting and more, the knees are essential parts of a healthy, active body.”
The Knee
Conditions of the knee
Anatomy of the Knee
The knee is a hinge joint made up of two bones, the thighbone (femur) and shinbone (tibia). There are two round knobs at the end of the femur called femoral condyles that articulate with the flat surface of the tibia called the tibial plateau. The tibial plateau on the inside of the leg is called the medial tibial plateau and on the outside of the leg, the lateral tibial plateau.
The two femoral condyles form a groove on the front (anterior) side of the knee called the patellofemoral groove. A small bone called the patella sits in this groove and forms the kneecap. It acts as a shield and protects the knee joint from direct trauma.
A fourth bone called the fibula is the other bone of the lower leg. This forms a small joint with the tibia. This joint has very little movement and is not considered a part of the main joint of the knee.
Articular cartilage and menisci of the knee
Movement of the bones causes friction between the articulating surfaces. To reduce this friction, all articulating surfaces involved in the movement are covered with a white, shiny, slippery layer called articular cartilage. The articulating surface of the femoral condyles, tibial plateaus and the back of the patella are covered with this cartilage. The cartilage provides a smooth surface that facilitates easy movement.
To further reduce friction between the articulating surfaces of the bones, the knee joint is lined by a synovial membrane that produces a thick clear fluid called synovial fluid. This fluid lubricates and nourishes the cartilage and bones inside the joint capsule.
Within the knee joint, between the femur and tibia, are two C-shaped cartilaginous structures called menisci. Menisci function to provide stability to the knee by spreading the weight of the upper body across the whole surface of the tibial plateau. The menisci help in load-bearing i.e. it prevents the weight from concentrating onto a small area, which could damage the articular cartilage. The menisci also act as a cushion between the femur and tibia by absorbing the shock produced by activities such as walking, running and jumping.
Ligaments of the knee
Ligaments are tough bands of tissue that connect one bone to another bone. The ligaments of the knee stabilize the knee joint. There are two important groups of ligaments that hold the bones of the knee joint together, collateral and cruciate ligaments.
Collateral ligaments are present on either side of the knee. They prevent the knee from moving too far during side to side motion. The collateral ligament on the inside is called the medial collateral ligament (MCL) and the collateral ligament on the outside is called the lateral collateral ligament (LCL).
Cruciate ligaments, present inside the knee joint, control the back-and-forth motion of the knee. The cruciate ligament in the front of the knee is called anterior cruciate ligament (ACL) and the cruciate ligament in the back of the knee is called posterior cruciate ligament (PCL).
Muscles of the knee
There are two major muscles in the knee - the quadriceps and the hamstrings, which enable movement of the knee joint. The quadriceps muscles are located in front of the thigh. When the quadriceps muscles contract, the knee straightens. The hamstrings are located at the back of the thigh. When the hamstring muscles contract, the knee bends
Tendons of the knee
A tendon is a tissue that attaches a muscle to a bone. The quadriceps muscles of the knee meet just above the patella and attach to it through a tendon called the quadriceps tendon. The patella further attaches to the tibia through a tendon called the patella tendon. The quadriceps muscle, quadriceps tendon, and patellar tendon all work together to straighten the knee.
Knee Arthritis
Evident Hip athritis in Xray
Image © American Academy of Orthopaedic Surgeons.
Arthritis simply means an inflammation of a joint causing pain, swelling, stiffness, instability and often deformity. Severe arthritis interferes with a person’s activities and limits his or her lifestyle.
Osteoarthritis or Degenerative Joint Disease - the most common type of arthritis. Osteoarthritis is also known as "wear and tear arthritis" since the cartilage simply wears out. When cartilage wears away, bone rubs on bone causing severe pain and disability. The most frequent reason for osteoarthritis is genetic, since the durability of each individual’s cartilage is based on genetics. If your parents have arthritis, you may also get it.
Trauma - can also lead to osteoarthritis. A bad fall or blow to the knee can injure the joint. If the injury does not heal properly, extra force may be placed on the joint, which over time can cause the cartilage to wear away.
Inflammatory Arthritis - swelling and heat (inflammation) of the joint lining causes a release of enzymes which soften and eventually destroy the cartilage. Rheumatoid arthritis, Lupus and psoriatic arthritis are inflammatory in nature.
Treatments for the knee
Total Knee Replacement Surgery
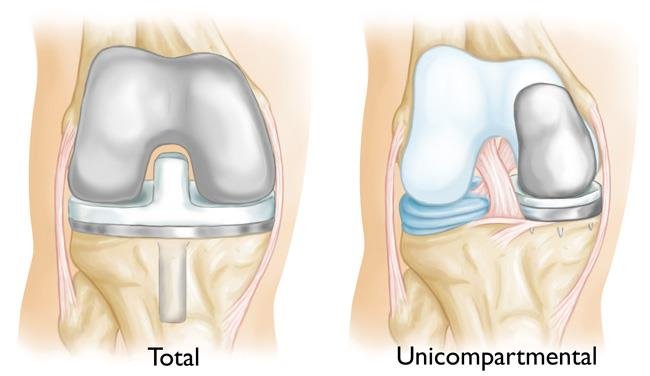
Total knee replacement is a surgical procedure in which the bone surfaces and cartilage that have been damaged or worn away are removed and replaced with artificial surfaces (‘implants’ or ‘prostheses’) made of metal or a plastic material. The resultant artificial joint is designed to move, as far as possible, like a natural healthy knee.
Model of a knee replacement
Your surgeon will advise which prototype will be best suited for you.
TOTAL KNEE REPLACEMENT VIDEO:
The animation below visually guides you through the process of a total knee replacement, a surgical procedure in which parts of an arthritic or damaged hip joint are removed and replaced with a metal, plastic or ceramic device called a prosthesis.
When Is Total Knee Replacement Recommended?
Several conditions can cause joint pain and disability and lead patients to consider joint replacement surgery. In many cases, joint pain is caused by damage to the cartilage that lines the ends of the bones (articular cartilage)—either from arthritis, a fracture, or another condition.
If nonsurgical treatments like medications, physical therapy, and activity modifications do not relieve your pain and disability, your doctor may recommend total joint replacement.
Preparing for Surgery
In the weeks before your surgery, your surgical team and primary care doctor will spend time preparing you for your upcoming procedure. For example, your primary care doctor may check your general health, and your surgeon may require several tests — such as blood tests and a cardiogram — to help plan your surgery.
There are also many things you can do to prepare. Talk to your doctor and ask questions. Prepare yourself physically by eating right and exercising. Take steps to manage your first weeks at home by arranging for help and obtaining assistive items, such as a shower bench, handrails, or a long-handled reacher. By planning ahead, you can help ensure a smooth surgery and speedy recovery.
Surgical Procedure
During the surgery, the damaged cartilage and bone is removed from your joint and replaced with prosthetic components made of metal, plastic, or ceramic. The prosthesis mimics the shape and movement of a natural joint. For example, in an arthritic hip, the damaged ball (the upper end of the femur) is replaced with a metal ball attached to a metal stem that is fitted into the femur, and a plastic socket is implanted into the pelvis, replacing the damaged socket.
Long-Term Outcomes
The majority of patients are able to perform daily activities more easily after joint replacement surgery. Most people can expect their joint replacement to last for many years, providing them with an improved quality of life that includes less pain, along with improved motion and strength that would not have been possible otherwise.
For more details on a total knee replacement CLICK HERE
Computer Assisted Orthopaedic Surgery
Computer assisted orthopaedic surgery (CAOS) is a minimally invasive surgical procedure, the surgeon replaces the hip joint with the aid of a computer guidance system. The system aids the surgeon in preparing and aligning the joint with the highest degree of accuracy.
CAOS has two basic components:
A special camera designed to see the surgical joint and limb and create a picture or image of the hip or knee
Computer programs which integrate these images with surgical information and assist the surgeon during the operation
CAOS can use actual images of the joint (X-Rays/fluoroscopic, ultrasound or CT images) or can create virtual images of the damaged joint. The camera and computer are given information by the surgeon about the normal and abnormal anatomic landmarks of the joint and limb. This information can be transmitted in several ways. Some CAOS systems use special cameras to identify and record the position of photo reflective spheres or infra-red light emitting devices. Some other systems use ultrasonic devises to identify bony landmarks. The surgeon uses the computer generated information and images to accurately and reproducibly reconstruct the damaged joint and limb.
Benefits
Potential benefits of using CAS/Robotics in joint replacement surgery include:
Computer organised and directed surgical work flow
Potential improved reliability of sizing and positioning of joint implants
Documentation of limb/joint anatomy and deformity
Data storage for research and outcome analysis
Potential improved accuracy of reconstructed limb length
Potential improved accuracy of prosthetic component alignment
Potential impact on functional outcomes and implant durability
Candidates for Surgery
While these technologies can be used in any patient, it is especially helpful in those patients who have specific bone deformities or have hardware from previous surgeries.
Robotic Assisted Total Knee Replacement
Arthroplasty means the surgical repair of a joint. Your surgeon performs an arthroplasty using metal and/or plastic parts to reconstruct degenerative, damaged, or arthritic joint surfaces in patients with severe arthritis who have failed nonsurgical treatment and have disabling function, limitation of activities of daily living, and severe pain.
An example of one of our Robotic-assisted total knee replacements
The robotic-assisted procedure is designed to help total knee patients experience a quicker recovery with less pain. Robotic instrumentation is used to properly align and balance the joint, two factors that can significantly affect overall stability and recovery.
Allowing the surgeon to measure and track the knee anatomy and plan the implant placement to best fit the specific patient. The plan is optimised to restore proper soft tissue balance and leg alignment, two critical factors to knee replacement outcomes. Robotic instruments are used by the surgeon with computer guidance to ensure the procedure is carried out precisely to plan.
Using these advanced robotics, the total knee replacement procedure is intended to help patients regain pain-free knee function, return to a normal daily lifestyle, and remain active for years to come.
Partial Knee Replacement
In unicompartmental knee replacement (also called partial knee replacement) only a portion of the knee is resurfaced. This procedure is an alternative to total knee replacement for patients whose disease is limited to just one area of the knee.
Your knee is divided into three areas: medial (inside of your knee), lateral (outside of your knee) and patella (kneecap/front of your knee).
Your orthopaedic surgeon can replace just the damaged area of your knee. This enables you to keep more of your natural bone, tissue and ligaments when compared with a total knee replacement (replacing two or three knee surfaces). A partial knee replacement is less invasive, which may afford you a faster recovery, less time in the hospital (1-2 days for a partial joint replacement compared with 3-4 days for a total joint replacement), and a more active life than with a total knee replacement.
There are a range of treatments for knee osteoarthritis, and your doctor will discuss with you the options that will best relieve your individual osteoarthritis symptoms.
Description
In knee osteoarthritis, the cartilage protecting the bones of the knee slowly wears away. This can occur throughout the knee joint or just in a single area of the knee.
The knee is divided into three major compartments:
Medial compartment (the inside part of the knee)
Lateral compartment (the outside part of the knee)
Patellofemoral compartment (the front of the knee between the kneecap and thighbone)
Image © American Academy of Orthopaedic Surgeons.
(Left) Illustration of a normal knee joint: The medial, lateral, and patellofemoral compartments are shown with red arrows. (Right) An X-ray of a normal knee joint showing healthy space between the bones.
Advanced osteoarthritis that is limited to a single compartment may be treated with a unicompartmental knee replacement. During this procedure, the damaged compartment is replaced with metal and plastic. The healthy cartilage and bone, as well as all of the ligaments, are preserved.
Image © American Academy of Orthopaedic Surgeons.
(Left) Illustration of osteoarthritis that is limited to the medial compartment. (Right) This X-ray shows severe osteoarthritis with bone-on-bone degeneration in the medial compartment (arrow).
Advantages and Disadvantages of Partial Knee Replacement
Multiple studies show that most patients who are appropriate candidates for unicompartmental knee replacement have good results with this procedure.
The advantages of partial knee replacement over total knee replacement include:
Quicker recovery
Less pain after surgery
Less blood loss
Lower risk of infection and blood clots
Also, because the bone, cartilage, and ligaments in the healthy parts of the knee are preserved, many patients report that a unicompartmental knee replacement feels more natural than a total knee replacement. A unicompartmental knee may also bend better.
The disadvantage of partial knee replacement compared with total knee replacement is the potential need for more surgery. For example, a total knee replacement may be necessary in the future if arthritis develops in the parts of the knee that have not been replaced. The need for additional surgery is slightly higher for partial knee replacement than for total knee replacement.
Image © American Academy of Orthopaedic Surgeons.
An advantage of partial knee replacement over total knee replacement is that healthy parts of the knee are preserved, which helps to maintain more natural function of the knee.
Candidates for Surgery
If your osteoarthritis has advanced and nonsurgical treatment options are no longer relieving your symptoms, your doctor may recommend knee replacement surgery.
To be a candidate for unicompartmental knee replacement, your arthritis must be limited to one compartment of your knee.
If you have any of the following characteristics, you may not be eligible for the procedure:
Inflammatory arthritis
Significant knee stiffness
Ligament damage
With proper patient selection, modern unicompartmental knee replacements have demonstrated excellent medium- and long-term results in both younger and older patients.
Orthopaedic Evaluation
A thorough evaluation by an orthopaedic surgeon will determine whether you are a good candidate for a partial knee replacement.
For more details on a partial knee replacement VISIT ORTHO INFO.
The freedom in being yourself… again
We understand you…. Text to motivate and show support from SOC. Call us today to discuss how we can help and improve you pain, Regain your freedom again.